What are risk factors for macular degeneration?
The greatest risk factor is age. Although AMD may occur during middle age, studies show that people over age 60 are clearly at greater risk than other age groups. Middle-aged people have about a 2% risk of getting AMD while people over age 75 have a nearly 30% risk.Other risk factors include smoking, obesity, white race, female gender, a family history of macular degeneration, a diet low in fruit and vegetables, high blood pressure, and elevated blood cholesterol.
What are macular degeneration symptoms?
Neither dry nor wet AMD cause any eye pain.The most common early symptom in dry AMD is blurred vision. As fewer cells in the macula are able to function, people will see details less clearly in front of them, such as faces or words in a book. Often this blurred vision will go away in brighter light. If the loss of these light-sensing cells becomes great, people may see a small black or gray blind spot in the middle of their field of vision.
Dry macular degeneration symptoms usually develop gradually and do not include total blindness. However, the symptoms may worsen the quality of life by making reading, driving, and facial recognition difficult Other symptoms may include decreased night vision, a decrease in the intensity or brightness of colors, increase in the haziness of overall vision.
Dry macular degeneration may affect one eye or both eyes. If only one eye is affected, symptoms may not be noticed because the unaffected eye has no visual symptoms.
All of the above symptoms may also be noticed in the wet form of AMD. In addition, the most common symptom in wet macular degeneration is straight lines appearing crooked or wavy. This results when fluid from the leaking blood vessels gathers within and lifts the macula, distorting vision. Larger areas of gray or black in the central area of vision may also occur. The central vision may decrease over a short period of time.
What are signs of macular degeneration?
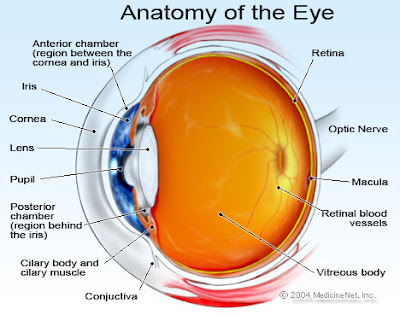
In both dry and wet forms of macular degeneration, the ophthalmologist may find decreased visual clarity (acuity) with preservation of peripheral vision and changes in the central retina visible with the ophthalmoscope.How is macular degeneration diagnosed?
Your ophthalmologist may suspect the diagnosis of AMD if you are over age 60 and have had recent changes in your central vision. To look for signs of the disease, he or she will use eyedrops to dilate, or enlarge, your pupils. Dilating the pupils allows your ophthalmologist to view the back of the eye better.Early AMD is often diagnosed during a comprehensive eye exam in patients without significant symptoms. This eye exam includes having drops placed in your eyes to enlarge, or dilate, the pupils. Your ophthalmologist will carefully examine the central portion of the retina to determine the presence or absence of AMD using various illuminating and magnifying devices.
During the eye exam, you may be asked to look at a checkerboard pattern called an Amsler grid. When looking at an Amsler grid with one eye, patients with AMD may notice that the straight lines of the checkerboard appear wavy or are missing.
Other diagnostic tests that your ophthalmologist may perform include retinal photography, fluorescein angiography and optical coherence tomography. All of these can help to differentiate between dry and wet forms of AMD and also document the abnormalities so that progression and response to treatment can be better measured.
What is the treatment for wet macular degeneration?
Wet AMD can be treated with laser surgery, photodynamic therapy, and injections into the eye. None of these treatments is a permanent cure for wet AMD. The disease and loss of vision may progress despite treatment.Laser surgery is used to destroy the fragile, leaky blood vessels. A high energy beam of light is aimed directly onto the new blood vessels to eradicate them, preventing further loss of vision. However, laser treatment may also destroy some surrounding healthy tissue and some vision. Because of this, only eyes with new vessels away from the exact center of the vision can be treated. This represents only a small proportion of patients with AMD. Laser surgery is only effective in halting or slowing visual loss if the leaky blood vessels have developed away from the fovea, the central part of the macula. Even in treated cases, the risk of new blood vessels recurring after treatment is significant and further or other treatment may be necessary.
Photodynamic therapy uses a drug called verteporfin (Visudyne) being injected into a vein of the arm. A light is then directed into the eye to activate the drug adhering to the blood vessels in the eye. The activated drug destroys the new blood vessels and leads to a slower rate of vision decline. Photodynamic therapy may slow the rate of vision loss. It does not stop vision loss or restore vision in eyes already damaged by advanced AMD. Treatment results often are temporary. Retreatment may be necessary.
Within the last seven years, injections into the eye with drugs specifically developed to stop the growth of new blood vessels have revolutionized the treatment of wet macular degeneration. We have learned that a specific chemical called vascular endothelial growth factor (VEGF) is necessary for the new blood vessels to grow under the retina. Drugs that counter VEGF (anti-VEGF pharmacotherapy) can be injected into the eye to arrest development of new blood vessels and sometimes cause them to regress. These drugs are injected in the ophthalmologist's office and may need to be given as frequently as monthly. Careful observation of the eye on a monthly basis to determine the drug effect is necessary. With this treatment, visual loss can often be halted or slowed and some patients will even experience some improvement of vision. Newer drugs currently under review may need to be given less frequently.
In patients with far advanced macular degeneration on both eyes, surgery to implant a telescopic lens in one eye is an option. The telescope implant, which surgically replaces the eye's natural lens, magnifies images while reducing the field of vision (peripheral vision). The telescopic lens implant may improve both distance and close-up central vision.
What is the treatment for dry macular degeneration?
There is currently no treatment available to reverse dry macular degeneration. However, dry macular degeneration is usually slowly progressive and most patients with this condition are able to live relatively normal, productive lives. Often one eye is affected more than the other.Once dry AMD reaches the advanced stage, no form of treatment can prevent further vision loss. However, treatment can delay and possibly prevent intermediate AMD from progressing to the advanced stage of severe vision loss. The National Eye Institute's Age-Related Eye Disease Study (AREDS) found that taking a specific high-dose formulation of antioxidants and zinc significantly reduces the risk of advanced AMD and it's associated vision loss. Slowing AMD's progression from the intermediate stage to the advanced stage is helpful in reducing the progression of visual loss in many people.
In this study, researchers used an antioxidant formulation that included vitamin C, vitamin E, beta carotene (or vitamin A), and zinc. For people with early-stage dry macular degeneration, there is no evidence that these vitamins provide a benefit. It is recommended that people with intermediate-stage dry AMD in one or both eyes or advanced stage AMD (dry or wet) in one eye, but not the other eye, take the AREDS formulation. Patients with increased risk of lung cancer should not take beta carotene. Studies involving other supplements such as lutein and bilberry are currently being performed.
The progression of dry age-related macular degeneration can also be slowed through lifestyle changes. These include changing the diet to include more fruits and vegetable, choosing healthy unsaturated fats, such as olive oil, over unhealthy saturated fats, such as butter, eating whole grains rather than refined grains and adding fish high in omega-3 fatty acids.
What are complications of macular degeneration?
Progression to wet macular degeneration is the main complication of dry age-related macular degeneration. At any time, dry macular degeneration can progress to the more severe form of the disease called wet macular degeneration, which may cause rapid vision loss. There's no accurate way to predict who will eventually develop wet macular degeneration.Other eye diseases such as cataracts, glaucoma, retinal detachment, or dry eyes are not complications of macular degeneration. Patients with macular degeneration can, however, develop these or other eye diseases.
What is the prognosis for macular degeneration?
Macular degeneration in its advanced form can cause loss of all central vision in both eyes. In the absence of other eye diseases, peripheral vision is maintained. Therefore, patients with advanced macular degeneration are, in most cases, able to see enough to get around in familiar situations.The use of magnifying devices can often improve vision in macular degeneration to allow for reading or watching of television.